Effect of diabetes on vision
Diabetes and vision
Diabetic eye disease is one of the most common causes of vision loss. The development and progress of diabetic retinopathy depend on the type of diabetes and the age, at which the patient falls ill with diabetes mellitus. Diabetic retinopathy can develop to any patient with diabetes of type 1 or type 2. It initially causes only minor vision impairments, but later is causing blindness, so regular doctor visits are essential to control the disease as much as possible and slow down its development.
Diabetic retinopathy
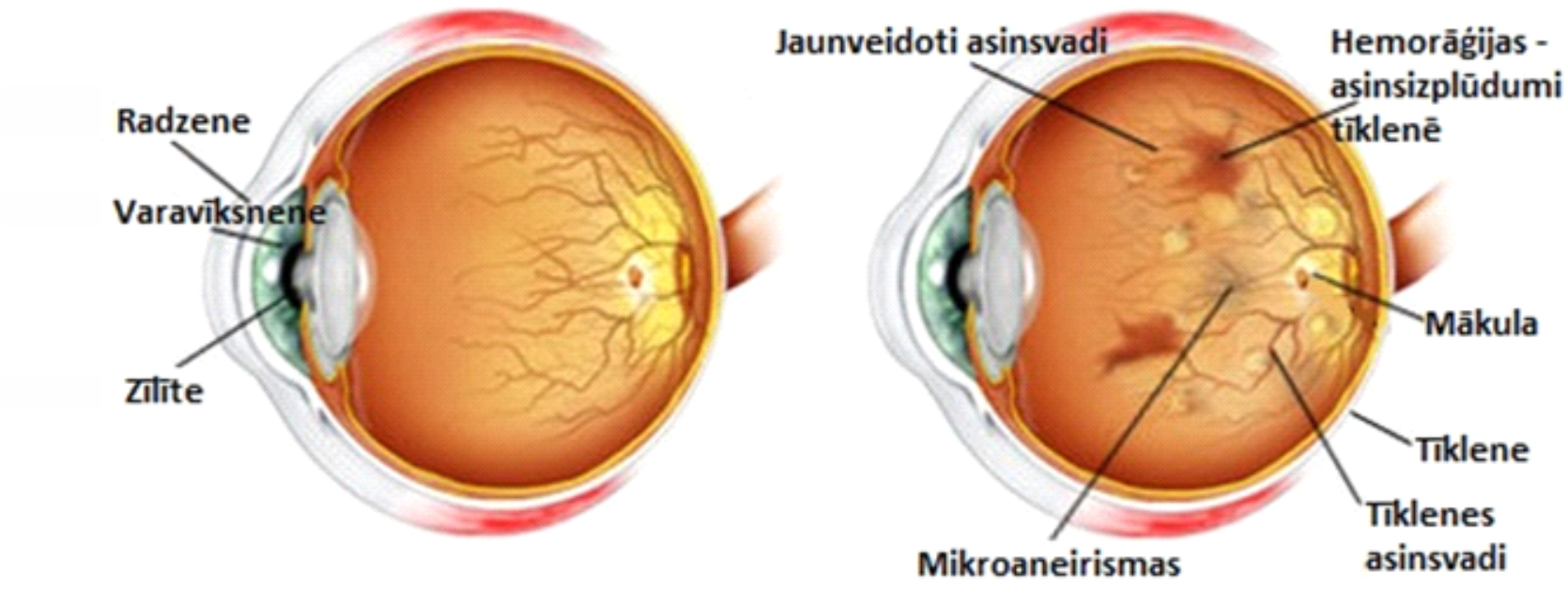
Normal eye Diabetic retinopathy
Radzene- Cornea
Varavīksnene – Iris
Zīlīte – Pupil
Jaunizveidotie asinsvadi – New blood vessels
Asinsizplūdumi tīklenē - Hemorrhages – bleeding in retina
Mākula – Macula
Tīklene – Retina
Tīklenes asinsvadi – Blood vessels in the retina
Mikroaneirismas - Microaneurysms
What will the patient complaint about in the case of diabetic retinopathy?
At the earliest stage, the disease does not cause any complaints, but as the disease progresses, it affects the vision severely. When retinopathy progresses, this may lead to complaints of floating spots, periodically blurred vision, which may be due to blood sugar fluctuations, image and line distortion, as well as gradual or sudden worsening of vision.
What happens in the eye at diabetic retinopathy?
The cause of diabetic retinopathy is the changes in the retinal blood vessels. At the beginning of the disease, there are enlargements in the blood vessels that appear in the retina in the form of small dots. Such altered blood vessels have increased wall permeability, so liquids and lipids can accumulate in the retina. Lipids and proteins accumulate in the retina, forming yellowish, well-defined aggregates called solid exudates.
At breakage of abnormal blood vessel walls, the retinal hemorrhages are formed. Over time, the hemorrhages may absorb and change their location in the retina.
The characteristic features of diabetic retinopathy are also the cotton wool spots occurred due to blockage of retinal blood vessels, creating areas of vascular insufficiency in the retina.
Due to blood supply disorders, retinal veins form loops and expand locally. Connections or shunts begin to form between the arteries and veins in the inner layers of the retina. Such altered blood vessels are called intraretinal microvascular abnormalities (IRMA).
With blood supply disturbances continuing, blood vessels begin to produce substances that promote the formation of new blood vessels, striving to restore normal blood supply to retinal area and its nourishing. However, newly developed blood vessels are fragile and often bleed, causing further additional hemorrhages in both the retina and on the optic nerve, as well as in the vitreous body.
How often should the ophthalmologist be visited if the patient is diagnosed with diabetes?
Every diabetic patient, even if there are no complaints about eye health, should attend the eye doctor at least once a year. Examination should be definitely made with a dilated (widened) pupil, since the changes caused by diabetes mellitus can be also found in the periphery of the retina. It is not possible to diagnose the changes inherent to diabetes and assess the periphery of retina with a narrow pupil.
How is diabetic retinopathy treated?
The successful treatment of diabetic retinopathy is based on well-controlled glucose and blood lipids, as well as a normalized blood pressure. These factors considerably slow down the progress of the disease. It is important to diagnose and initiate diabetic retinopathy treatment in a timely manner. If changes in the disease affected the macula of the central part of the retina, visual acuity can be significantly reduced. If diabetic retinopathy changes not affected the retinal center, retinal laser photocoagulation is indicated in the treatment with the aim of eliminating newly developed blood vessels and areas of retinal ischaemia, thereby reducing the progress of the disease.
However, if the disease is progressed and / or the retinal edema developed, the drugs of the vascular endothelial growth factor inhibitor group (Anti-VEGF) that inhibit the formation of newly developed blood vessels and reduce retinal edema are injected into the eye.
Intravitreal injection of medication